Risk assessment plays an important role within the dynamic field of nursing and patient safety. As caregivers and advocates, nurses typically navigate complex challenges highlighted by diverse risk aspects. And amidst these pressures, managing stress becomes essential for maintaining well-being and providing optimal care.
This comprehensive guide goes into the core suggestions and practical advice geared toward empowering nurses to master risk evaluation while also offering invaluable strategies to alleviate stress and seek vital support. From understanding prevalent risk aspects to fostering resilience and collaborative solutions, this resource equips nurses to thrive while prioritizing their mental and emotional health.
Understanding risks in healthcare
Risk assessment is an in depth evaluation by medical professionals of what might adversely affect individuals to judge if adequate precautions are in place or in the event that they should do more to forestall harm. Healthcare experts gather detailed information on patients’ health, physical problems, and risk aspects as a part of the evaluation process to discover possible vulnerabilities.
Nurses are all the time on the forefront of healthcare, placing them able to handle various risks. These risks typically extend beyond clinical difficulties, including environmental, genetic, ethical, and social elements. By thoroughly reviewing these aspects, nurses can proactively discover, evaluate, and eliminate hazards prematurely, providing higher care.
Environmental risks
Certain physical, chemical, biological, and psychosocial elements affect individuals’ and communities’ overall health and well-being. These elements are known as environmental risks. Some prevalent examples of environmental risks include air pollution, water contamination, contagious illnesses, noise pollution, stress, climate-related hazards, and, in some cases, violence.
Quite a few health issues are connected to elements inside the environment. Yet, the scope of those health concerns extends beyond mere exposure to those elements. Environmental risks may end up in a cascade of biological events that alter how the body works. While the consequence is primarily adversarial, environmental aspects could also end in good change, depending on genes and circumstances.
Nonetheless, medical professionals must evaluate these risks and address them through comprehensive measures and protocols when vital. Over time, healthcare professionals have developed strict infection control practices, improved cleanliness and waste management in communities, and provided adequate training that improves safety regulations across diverse healthcare systems.
Prioritizing such measures helps to limit environmental risks, improve patient health, and protect healthcare employees.
Genetic risks
Genetic risk is the probability of an individual developing a disease or health condition based on their genetic makeup. Medical professionals determine this by the presence or absence of specific genetic elements related to these health conditions.
In response to the Third National Health and Nutrition Examination Survey, many individuals within the US population have polymorphisms of their genes, which may affect their health. Because of this, genomic testing has change into a prevalent practice for identifying genetic risks and diagnosing rare diseases.
Moreover, it underscores the importance of nurses acquiring fundamental training in genetics and genomics. Proficiency in these areas enables them to deliver care to those impacted or liable to genetic conditions. With a solid understanding of those concepts, nurses are higher equipped to help patients and their families in comprehending the importance of genetic testing, counseling, and other therapeutic options.
Ethical risks
Ethical risks encompass moral distress and uncertainties stemming from different values, beliefs, and interests in healthcare decisions and practices. These risks commonly arise in contexts comparable to end-of-life care, informed consent, patient confidentiality, and instances of research misconduct. In essence, ethical risks entail navigating intricate moral dilemmas which have extensive implications for patients, healthcare professionals, and the medical system.
Because of this of their interaction with patients, nurses often face ethical risks, and there may be a must apply moral reasoning and decision-making skills to discover the very best outcomes for every situation. Ethical risks are sometimes addressed through ethical frameworks, codes of conduct, and skilled standards. These strategies help uphold nurses’ moral responsibilities to each healthcare stakeholder.
Social risks
Every social, cultural, economic, and political factor able to significantly impacting healthcare services’ access, quality, and consequence is grouped under social risks. Social risks typically range from poverty to stigmatization, discrimination, marginalization, and human rights violations, to say a couple of.
Nurses address these social risks by working to advertise health equity, diversity, and inclusion. In addition they advocate for social justice across the community they serve. It’s common for nurses to collaborate with community members, healthcare professionals, and policymakers to implement social policies and programs able to improving the health and wellness of vulnerable populations.
Strategies for assessing risks in nursing practice
There are different methods and tools for risk assessment and evaluation, depending on the context and scope of the situation. Nevertheless, nurses can follow some general steps to judge diverse healthcare risks accurately.
Patient assessment
Before nurses engage in any medical intervention, they have to thoroughly assess the patient’s condition, medical history, and current status. This process helps to find out all of the vital information to develop effective risk management strategies.
The assessment process involves defining the aim and criteria for the chance evaluation. On account of the collaborative nature of healthcare, it’s also essential to ascertain the roles of everyone involved. Nurses can then collect and record details about risk sources, causes, and consequences.
Risk prioritization
A vital element of risk management is prioritization. In reality, not all risks carry the identical severity levels, and nurses must rank risks based on their potential impact. Higher priority risks are subjected to more critical preventive measures and prompt interventions.
Once risks have been ranked, nurses can select a response by comparing them with established criteria grounded on evidence-based practice and choosing probably the most appropriate technique to take care of them. Some prevalent methods for this step include avoiding, transferring, reducing, or accepting the risks, depending on the context.
Utilizing evidence-based practices
Evidence-based practices have change into a mainstay in modern healthcare, significantly impacting healthcare quality, safety, and efficacy. Integrating these practices has also caused a positive change in healthcare delivery by highlighting the usage of probably the most current and reliable evidence.
Nurses may also depend on these practices to base their interventions on current research and proven methodologies. With this approach, nurses can minimize the potential risks of outdated or ineffective treatments.
Evaluation
After establishing and prioritizing the risks, the subsequent step is performing quantitative and qualitative evaluation. Qualitative risk evaluation typically requires risk matrices, scoring systems, or other rating methods to categorize and prioritize risks.
Alternatively, quantitative evaluation involves decision trees, sensitivity evaluation, or Monte Carlo simulation to ascertain the probability and impact of risks. These analyses also develop the consequences of risks on the outcomes and objectives of healthcare.
Adherence to protocols
Protocols are fundamental pillars in healthcare, designed to enhance the general standard of patient care in any clinical setting. It breaks down essential medical components, comparable to risk assessment, making it easier for nurses to administer and reduce patient harm.
Every healthcare skilled recognizes the necessity to follow established protocols and standards. These guidelines help to mitigate risks and guarantee a uniform and standardized approach to delivering patient care.
Effective communication
Open communication is crucial for healthcare professionals to share vital details about a patient’s condition, treatment plan, and prognosis. It also allows for effective collaboration between different healthcare team members, which is important for providing coordinated and comprehensive care.
As such, it’s imperative that nurses adeptly communicate with fellow healthcare professionals, patients, and their families. Within the context of risk assessment, adequate communication guarantees comprehensive awareness and alignment amongst all involved parties regarding the patient’s care plan.
Continual education and training
Nursing is a dynamic field, and staying updated with the newest advancements, techniques, and best practices is crucial. Regular education and training sessions empower nurses to adapt to recent challenges and implement safer care practices.
Marymount University allows professionals to match ABSN vs. BSN programs online and select which they like. Traditional BSN programs work well for college students pursuing their first college degrees, while ABSN programs are tailored toward career-changing professionals with bachelor’s degrees in non-nursing disciplines. In either case, each programs offer optimal pathways to becoming registered nurses and implementing effective strategies for risk evaluation and other medical procedures. Students can find out how the healthcare system, research, education, and society relate to mental health and mental illness.
Continuous monitoring and evaluation
Finally, monitoring and reviewing the risks and risk responses is vital. This step involves tracking and measuring the performance and effectiveness of the chance management process and making appropriate adjustments when needed.
Regular monitoring allows nurses to discover any changes in patient condition promptly. This constant vigilance helps evaluate the effectiveness of ongoing treatments and interventions, thereby mitigating risks related to unexpected complications.
Advantages and challenges of risk assessment
The trendy healthcare landscape emphasizes risk assessment for reason. By conducting risk assessments, nurses can enhance patient satisfaction and trust by involving them within the assessment and evaluation process. In addition they change into more expert in communicating the risks and the chance response clearly and transparently.
As expected, the chance assessment process enhances nurses’ ability to acknowledge potential or existing risks that might impact their patients. This permits them to implement preventative or remedial measures as needed and improve the standard and safety of care by mitigating the likelihood and impact of adversarial events, errors, or complications.
Finally, risk evaluation demonstrates skilled competence and accountability by following evidence-based practice and ethical standards.
Nevertheless, despite these advantages, risk assessment and evaluation may also pose challenges for nurses. Typically, nurses take care of uncertainty and complexity as risks change over time and will be influenced by multiple aspects and interdependencies. Risk response can also require additional resources, time, and energy.
It could actually even be difficult to administer the emotional and psychological elements of risk evaluation. Sometimes, the method involves facing difficult and stressful situations; at other times, nurses are tasked with making tough or controversial decisions. How, then, can they overcome these challenges? That is where coping mechanisms change into relevant.
Essential coping mechanisms for nurse stress relief
Stress is probably the most impactful yet ignored issues in nursing. Most of the time, healthcare’s emotional and physical demands change into so overwhelming that they affect many elements of nurses’ work and private lives.
The impact of stress is well known in healthcare, a lot in order that it has been tagged an occupational hazard. Subsequently, coping with stress is crucial for an efficient and enjoyable profession. Listed here are some coping mechanisms nurses can prioritize to alleviate stress.
Maintain a routine
Routines are effective in keeping people organized and structured, two habits which can be crucial for each nurse. Developing a pattern will be especially vital during stressful times, providing you with a way of control, improving your focus, and increasing overall productivity.
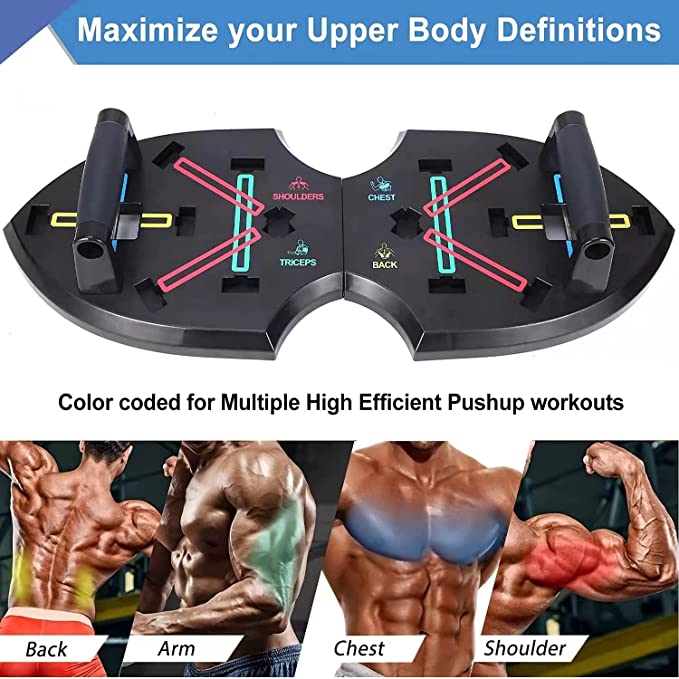
Exercise often
As a nurse, you likely walk for miles on every shift. Nevertheless, exercise outside work also has its advantages. Several studies have confirmed the healing advantages of physical exertion and the impact of physical activities on mental health, effectively addressing eating disorders, stress, anxiety, and depression. Moreover, regular workouts help release endorphins and improve sleep quality.
Good sleep
The importance of excellent sleep can’t be overstated. Research has shown that sleep helps rest and de-stressing and reduces the risks of mental ailments comparable to dementia. Nurses must prioritize their sleep and create a conducive environment that helps to foster good sleep.
Practice mindfulness
Mindfulness meditation is a mental training practice that teaches you to decelerate racing thoughts, let go of negativity, and calm your mind and body. Stress and depression are primarily rooted in concerns over what might occur, and mindfulness might help combat these feelings. Mindful practices involve respiration exercises, guided imagery, and other activities that loosen up the body and mind.
Prioritize self-care
The complex nature of nursing practice poses challenges for professionals in managing their well-being and mental health. This underscores the importance of self-care. Once you’re feeling overwhelmed, it’s time to implement rest or stress-reduction techniques to assist loosen up, regain focus, and promote overall well-being. Some self-care practices include progressive muscle rest, yoga, exercise, music and art therapy, aromatherapy, and cognitive-behavioral therapy, to say a couple of.
Nurses consistently face several stressors, from having to think critically to serving in an under-resourced or understaffed environment. Hence, it’s all the time good practice to implement mechanisms that help them deal with stress.
Looking for support: Who to show to when managing high-stress situations
While nurses are adept at handling stressful situations, we must acknowledge that searching for support and guidance during heightened stress is significant to self-care and skilled growth. Knowing who to show to for help can significantly impact a nurse’s coping ability. Listed here are several avenues for searching for support in high-stress scenarios:
Supervisors and managers
Every medical and non-medical facility has leaders who help guide, advise, and support other employees. Nurses can make the most of this useful resource each time they face high-stress situations. Moreover, supervisors and managers can offer resources or additional assistance when needed.
Mental health professionals
Looking for support from mental health professionals, comparable to counselors or therapists, will be hugely useful. Mental health professionals are well-equipped to assist nurses develop coping strategies, stress management techniques, and a secure space to debate the emotional toll of high-stress situations.
Colleagues
The support from colleagues inside knowledgeable network holds immense value, especially in industries that emphasize collaboration and teamwork. Fellow healthcare professionals understand the difficulties encountered and may offer empathy, exchange experiences, and extend emotional support during difficult periods.
Skilled networks
Engaging with skilled nursing associations or networks can offer access to support groups, forums, and resources specifically designed to help nurses in managing stress and difficult situations.
Worker assistance programs (EAPs)
Worker assistance programs are work-based initiatives that help employees address personal issues. Many healthcare firms have EAPs, which provide confidential counseling services, tools, and support to staff experiencing stress or burnout.
Personal support networks
Finally, personal support networks comparable to friends and families are also crucial. They provide a way of comfort, understanding, and a non-professional perspective that will be uplifting during difficult times.
The vital role of risk evaluation
While risk evaluation and other medical procedures are vital, we must also recognize the toll they will tackle nurses’ well-being. Hence, understanding the necessity for support and where to hunt it is important for nurses in managing high-stress situations. Moreover, healthcare organizations also needs to provide accessible resources to support nurses’ mental and emotional health.