Infection of joint prostheses is a comparatively frequent complication following joint replacements. Prosthesis placement is a really widespread surgery nowadays, which helps to treat quite a few pathologies related to the bone apparatus.
A lot of the cases involve hip or knee prostheses. Although they’re procedures with superb results, they’ll have complications, as with every other surgical technique. Why does this infection occur? What are its symptoms? Below, we’ll answer these questions.
What’s joint prosthesis infection?
Joint prosthesis infection can also be often called ‘periprosthetic infection’. It’s a complication that compromises each the joint alternative area and the adjoining tissues.
Arthroplasty is the medical name for this procedure. In response to information from the University of Navarra Clinic, around 30,000 interventions of this sort are performed in Spain every yr. It is a secure procedure that, generally, produces a notable improvement within the patient’s quality of life.
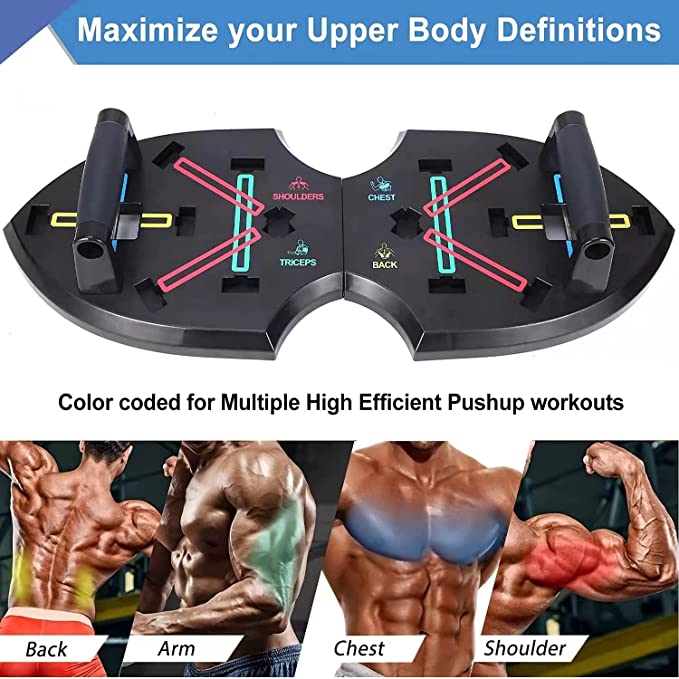
The joints most definitely to get replaced by a prosthesis are the hip and the knee.
Even so, as stated in a publication in Clinical Microbiology Reviews, a minority of patients will experience device failure and require additional surgery in some unspecified time in the future of their lives. It’s estimated that 2-4% of arthroplasty cases lead to infection.
The large problem is that it might cause other serious complications, in addition to high costs to the healthcare system. In itself, it’s normally attributable to the patient’s own bacteriawhich form a gelatinous matrix on the prosthesis.
What happens is that these microorganisms adhere to the surface of the prosthesis. Once there, they multiply and provides rise to this matrix, which known as a biofilm. It is a mechanism that defends them from the motion of antibiotics, making them more immune to treatment.
Why can joint prosthesis infection occur?
Infection of joint prostheses might be attributable to various kinds of bacteria. As now we have identified, they adhere to the prosthesis and form a biofilm. To do that, they organize themselves in layers, one on top of the opposite. This explains why those present in the deeper layers are more immune to antibiotics.
Nevertheless, the prosthesis itself also alters the function of certain cells of the immune system, reminiscent of phagocytes. All these aspects favor the progression of the infection and make it difficult to treat.
The bacteria normally involved are staphylococci. Inside this group, essentially the most frequent microorganisms are Staphylococcus aureus and Staphylococcus epidermidis. Other agents involved are the next:
- Escherichia coli
- Pseudomonas aeruginosa
- Enterococcus spp
It can also be a polymicrobial infection. That’s, it could be attributable to a couple of bacterium. Fungal infections are less frequent.
We predict you might be involved in reading this, too: Joint Hypermobility Syndrome: What Is It and How To Deal With It?
Kinds of infection
Infection of joint prostheses is generally classified in keeping with the time of evolution. Some authors distinguish between acute and chronic infection. Nevertheless, as explained within the Prioam Guideit might even be classified as follows
- Early postoperative infection (PPI)
- Late chronic infection (LCI)
- Acute hematogenous infection (AHI)
Those that only distinguish between acute and chronic infection include acute hematogenous infection in the primary group.
Early postsurgical infection or acute infection
Early postsurgical infection is that which occurs in the primary month after prosthesis placement. Some consider that it’s still considered acute infection up to a few months after surgery.
There are a series of criteria that help to discover this kind of joint prosthesis infection. There is generally dehiscence and suppuration of the surgical wound. As well as, when fluid is faraway from the joint and examined within the laboratory, the presence of bacteria is commonly detected.
In these cases, early diagnosis and treatment are essential. In this fashion, the necessity to switch the prosthesis resulting from infection might be avoided.
Acute hematogenous infection
Acute hematogenous infection occurs when the main focus of infection is elsewhere within the body. In other words, the bacteria can come from one other process reminiscent of pneumonia, urinary tract infection, endocarditis, etcetera. What happens is that they’re mobilized with the blood and find yourself colonizing the prosthesis.
Infection of an articular prosthesis of chronic type
A chronic infection is generally considered when three months have passed from the position of the prosthesis. It’s more complicated to treat than acute ones, since the bacterial biofilm has matured and can’t be removed.
This condition evolves progressively and insidiously. Pain persists for months, although there aren’t any clear signs of infection or fever. In some cases, abscesses and fistulas could also be present. In these cases, alternative of the prosthesis is generally needed.
Associated symptoms
The symptoms of joint prosthesis infection vary depending on whether or not they are acute or chronic. It’s essential to notice that about half of the cases are chronic. Due to this fact, one in all the predominant symptoms is inflammatory pain.
The issue is that arthroplasties may cause pain without necessarily causing infection. Hence, it’s sometimes difficult to achieve an accurate diagnosis. Along with pain, there could also be a scarcity of functionality within the joint.
In cases of acute infection, patients normally present fever. The surgical wound doesn’t heal properly and there could also be oozing of purulent material through the wound. The world is generally swollen, warm, and red.
Like this text? Chances are you’ll also wish to read: Joint Effusion: What Is It and How Can It Be Treated?
How is joint alternative infection diagnosed?
The diagnosis of this kind of infection ought to be made early. This prevents the infection from becoming chronic and the operation from having to be repeated. With the intention to accomplish that, it’s essential to watch the patient properly and to be attentive to any warning signs.
Nevertheless, there are plenty of complementary tests that might help within the diagnosis. Certainly one of these is positron emission tomography. It is a technique that uses a glucose tracer. This molecule is captured by the bacteria causing the infection.
Thus, by way of the scan, the areas where the bacteria are situated might be appreciated. Other useful tests are synovial fluid evaluation and blood tests. Ultrasounds and X-rays can be useful.
Available treatments
Infection of joint replacements requires multidisciplinary treatment. In all kinds, medical and surgery is generally combined. The medical treatment is predicated on reducing pain and administering specific antibiotics to cure the infection.
Surgery might be used to wash and debride the tissues. In cases where the infection is chronic, prosthesis alternative is prone to be required. This might be done as a one-stage or two-stage procedure.
That’s, the brand new prosthesis might be placed in the identical surgery. The 2-stage option involves removing the prosthesis, cleansing the realm, and placing a spacer containing antibiotics. Then, in one other operation, the brand new prosthesis is placed.
With the intention to establish antibiotic treatment, it’s advisable to first discover the causative germ and its sensitivity to those drugs. The duration of treatment might be long. In some cases, reminiscent of knee prostheses, six months of treatment could also be advisable.
Remember: An infection of joint prostheses might be serious
Although this isn’t a quite common complication, an infection of prostheses could be very feared by surgeons. It is because in some cases it requires further surgery and alternative of the prosthesis.
It’s essential for patients to pay attention to the signs and symptoms with the intention to give you the chance to discover an infection early. As well as, physicians should make the diagnosis as quickly as possible, as this reduces the likelihood of needing to operate again.
It would interest you…